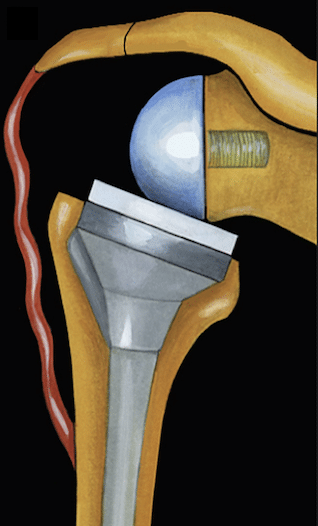
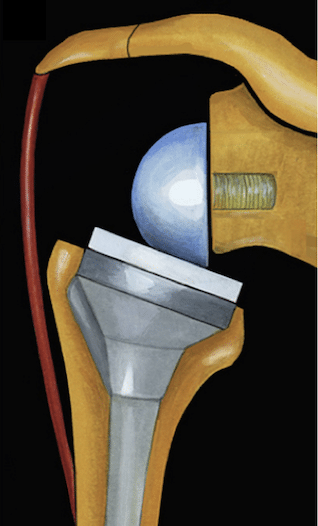
Reverse means the opposite. While non-reverse prostheses are referred to as “anatomical prostheses,” reverse prostheses are considered “non-anatomical” prostheses. In anatomical prostheses, the shoulder joint is completely mimicked or replicated. Despite being anatomical, they depend on the integrity of the rotator cuff muscles’ sleeve to functionally operate the shoulder joint. The humeral head (the ball) is made of cobalt-chromium or titanium, and it is placed into the polyethylene (soft) socket (Figure 1).


In reverse prostheses, the design logic works differently. The main objective of these types of prostheses is to enable the lifting of the arm from the shoulder joint by utilizing the assistance of the deltoid muscle when the rotator cuff, also known as the rotator cuff muscles, is not functioning or has suffered irreparable damage. The humeral head is replaced with the socket of the shoulder, essentially transforming the original socket into the humeral head, and the humeral head becomes the socket of the shoulder.
Reverse prostheses were initially designed as a salvage prosthesis for irreparable tears of the shoulder muscles and permanent degeneration of the shoulder joint in older individuals. However, in recent times, they have also become widely used for severely fragmented fractures of the humeral head in advanced age groups, where repair is not feasible.

Another requirement of reverse prostheses is that previously applied prostheses (partial or total – anatomical) are not functioning properly.



In reverse prostheses, the tension of the deltoid muscle, also known as the lateral muscle of the arm, is of utmost importance.

When the deltoid muscle is adequately tensioned after reverse prosthesis, patients will be able to lift their arm smoothly over their head.


Reverse prostheses are generally used in patients over 70 years old. Their use is limited in younger patients. This is due to the unknown durability of the prosthesis and the higher risk of complications in this age group due to increased activity levels.
In cases where reverse prosthesis cannot be performed due to reasons such as low bone stock and quality in advanced age or infection, it is recommended to remove the humeral head and leave the shoulder in a flail shoulder state.

Preoperative Preparation and Discharge
After the decision for surgery is made, consultations with other specialists (cardiology, internal medicine, etc.) may be requested by your anesthesiologist. If not already done, a computed tomography (CT) scan of the shoulder will be requested to assess bone stock and for surgical planning. The surgery is performed under general anesthesia and typically takes about 2 hours. This 2-hour period includes the time for induction and preparation (positioning, sterilization procedures, patient draping, etc.), which takes approximately 1 hour, and an additional hour for the awakening period after the surgery. It will generally take about 4 hours for you to leave your room and return to your room. However, if your surgery involves the correction of a previous procedure (revision), it may take significantly longer. Your hospital stay after the surgery will be an average of 2-3 days. During this time, you will be administered strong pain medication, receive ice application, dressing changes, and undergo ambulation. If necessary, blood transfusion may be administered to normalize general parameters. Once your overall condition and wound have improved, you will be discharged and instructed to take oral pain medication and antibiotics while walking.
Postoperative Care after Reverse Prosthesis
Compared to anatomical prostheses, dislocation is more common with reverse prostheses. Therefore, for at least 6 weeks after the surgery, it is important to avoid bringing the arm close to the body and rotating it inward. Rising from a chair with hands placed on the edges should be avoided as an undesirable example. Below are incorrect and correct movements (incorrect – correct) illustrated:
The shoulder-arm sling (with a waist belt) should be used for approximately 3-4 weeks. The link for the use of shoulder-arm sling is provided here: (https://youtu.be/FYqi0wgMQrI) on the side.
Remember to start removing your clothing from the non-operated arm, and lastly, remove the clothing from the operated arm. When putting on clothing, start with the operated arm first and then proceed in the reverse order.
You should have professional dressings done approximately 4-5 times. Within 3-4 days after the surgery, the wound dressing can be washed with lukewarm and gentle water.
During the first 6 weeks, you will have a check-up every 15 days for physical therapy education and wound observation. Afterwards, with the help of X-rays and a physical therapy program, you will gradually transition back to daily activities. The active lifting of your arm, similar to your preoperative movements, surgery, and the subsequent recovery process, will vary from person to person but typically takes an average of 6-8 weeks.





